When I first heard about adenomyosis, it was from a friend who had been struggling with painful periods for years. At first, she thought it was just “normal” discomfort until the symptoms became unbearable. After months of searching for answers, she finally got a diagnosis. It was a relief but also left her with so many questions about why it happened in the first place.
This experience made me realise how important it is to understand the root causes of adenomyosis. I’ve since worked with many women dealing with this condition, and I know how crucial it is to have reliable information. As a nutrition coach certified by the Institute of Integrative Nutrition in New York, I’m passionate about helping women take control of their health.
The root cause of adenomyosis is not fully understood. Current research points to factors such as hormonal imbalances, genetic predispositions, and environmental influences. Stress, past uterine surgeries, and diet may also contribute, but the condition is likely the result of a combination of factors.
What is Adenomyosis?

Adenomyosis is a condition where the tissue that lines the uterus (endometrium) grows into the muscular wall of the uterus. This abnormal growth can cause the uterus to thicken and enlarge, leading to symptoms such as heavy menstrual bleeding, intense cramping, and pelvic pain.
Adenomyosis is often confused with endometriosis, as the two share overlapping symptoms. However, the difference between adenomyosis and endometriosis lies in the tissue’s location. While adenomyosis occurs within the uterine wall, endometriosis involves tissue growing outside the uterus, often affecting the ovaries and surrounding organs. Both conditions may stem from similar hormonal or inflammatory factors.
Can Hormonal Imbalances Trigger Adenomyosis?

Hormonal imbalances, particularly involving oestrogen, are considered a significant factor in adenomyosis. Oestrogen promotes the growth of endometrial tissue, which may explain why adenomyosis is most prevalent during a woman’s reproductive years. This hormonal connection also raises questions about the potential role of environmental factors like endocrine-disrupting chemicals found in plastics or certain cosmetics.
Think of oestrogen as that overly enthusiastic gardener who doesn’t know when to stop pruning and planting. It means well but might just be doing too much in all the wrong places.
While not entirely proven, oestrogen dominance—a condition where oestrogen levels outweigh progesterone—may exacerbate adenomyosis. Reducing exposure to synthetic hormones and maintaining a healthy hormonal balance through diet and lifestyle changes can be beneficial in managing symptoms.
Is There a Genetic Link to Adenomyosis?
Research indicates that genetics may influence the likelihood of developing adenomyosis. Women with a family history of uterine conditions, such as endometriosis or fibroids, appear to be at greater risk. However, no single gene has been identified as the cause, and it’s likely that multiple genetic and environmental factors interact.
In some cases, adenomyosis may co-occur with autoimmune disorders, further suggesting a possible genetic or immune link. However, much of this connection remains theoretical, requiring more research to understand how genetics influence this condition.
How Do Lifestyle and Environmental Factors Contribute to Adenomyosis?

Lifestyle and environmental factors may indirectly contribute to the development of adenomyosis by affecting hormonal balance and inflammation. For example:
- Diet and Inflammation: Highly processed foods, refined sugars, and trans fats can increase inflammation, potentially worsening symptoms. In contrast, anti-inflammatory foods like fatty fish, leafy greens, and nuts may help reduce discomfort.
- Stress and Exercise: Chronic stress disrupts hormone regulation, while moderate exercise can reduce inflammation and improve overall well-being.
- Environmental Toxins: Endocrine-disrupting chemicals (EDCs) found in plastics, pesticides, and some personal care products may mimic oestrogen in the body, disrupting hormonal balance over time.
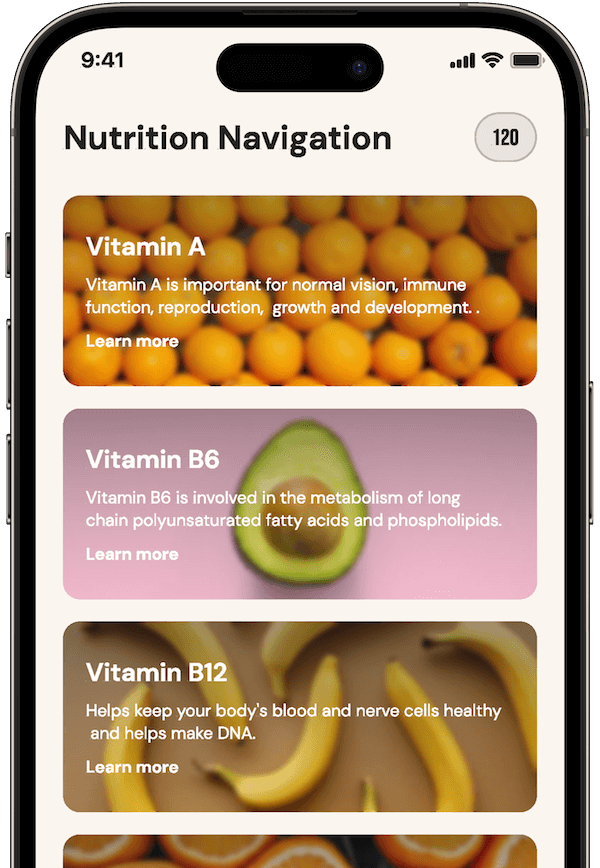
Tracking these factors can help women identify patterns that worsen or alleviate symptoms. That’s why I developed the Unprocessed App—a tool to help you monitor diet, stress, and overall well-being. It empowers you to take control of your health by understanding what works for your body. You can join the waitlist here.
Can Previous Uterine Surgeries Increase the Risk?

Previous uterine surgeries, such as C-sections, dilation and curettage (D&C) procedures, or fibroid removal, may increase the risk of developing adenomyosis. These procedures can disrupt the integrity of the uterine lining, potentially allowing endometrial cells to embed themselves into the uterine muscle wall.
However, not all women who undergo such procedures develop adenomyosis. This suggests that additional factors—such as hormonal imbalances or genetic predispositions—likely play a role. It’s a combination of these factors that makes identifying a single “cause” so challenging.
Is Adenomyosis a Result of Multiple Factors?
Adenomyosis is not caused by a single factor but rather a complex interaction of genetics, hormonal imbalances, inflammation, and external triggers like surgery or environmental toxins. Each of these elements contributes differently depending on a person’s unique biological and environmental history.
For example, someone with a genetic predisposition may not develop adenomyosis unless external factors, such as stress or uterine trauma, come into play. This layered approach to understanding adenomyosis highlights the importance of holistic management strategies, tailored to address multiple potential causes.
What are the Common Symptoms and Associated Risks?

Adenomyosis is characterised by heavy periods, pelvic pain, and cramping. However, it can also lead to:
- Adenomyosis Belly: An enlarged uterus can create a bloated or swollen appearance, often referred to as “adenomyosis belly”. This can be physically uncomfortable and affect self-esteem.
- Bowel Issues: Pressure from an enlarged uterus may cause gastrointestinal symptoms like bloating, constipation or diarrhoea.
- Weight Changes: Hormonal imbalances linked to adenomyosis can sometimes cause weight gain or difficulty maintaining a stable weight.
These symptoms can have a significant impact on daily life, which is why understanding the root causes and seeking effective management strategies are so crucial.
FAQs
Can adenomyosis cause anaemia?
Yes, adenomyosis can cause anaemia due to prolonged or heavy menstrual bleeding, which lowers iron levels in the body. This can lead to symptoms like fatigue, weakness, and dizziness.
Does adenomyosis affect menopause?
Adenomyosis symptoms often diminish after menopause, as oestrogen levels naturally decline, reducing tissue growth.
Is adenomyosis linked to miscarriages?
Research suggests adenomyosis may increase the risk of miscarriage in some women, likely due to changes in the uterine lining.
How long does it take to diagnose adenomyosis?
Diagnosing adenomyosis can take months or even years because symptoms often mimic other conditions like fibroids or endometriosis.
What imaging tests are most accurate for adenomyosis?
MRI is considered the most reliable imaging test for diagnosing adenomyosis, followed by transvaginal ultrasound.
Closing Thoughts
Living with adenomyosis can be overwhelming, but understanding its root causes offers hope. While the exact mechanisms remain unclear, learning about the hormonal, genetic, and environmental factors that contribute to this condition empowers you to take action.
If you’re ready to take control of your health, I encourage you to try tools like my Unprocessed App. Designed to help women track their diet, symptoms, and well-being, it offers insights that can make a real difference. Join the waitlist to start your journey toward better health. Remember, you’re not alone in this—together, we can navigate these challenges and work towards brighter, healthier days ahead.



